-
17e
CHAPTEROsteocalcin: New Frontiers in Diabetes
Sudha Vidyasagar, Avinash Holla
ABSTRACT
Osteocalcin (OCN) is a bone-derived hormone that has been found to decrease insulin resistance and improve β-cell function. The effects of OCN go beyond the control of blood sugars and may have a role in preventing micro and macrovascular complications of diabetes. This may make it an exciting target for the evolution of newer drugs in diabetes. In this chapter, we explore the evidence for OCN in human studies.
INTRODUCTION
The pathophysiology of type 2 diabetes mellitus (T2DM) has always been complicated. Described by DeFronzo, as the ominous octet, we know that there are missing links, as many more mechanisms have been proposed. One of these is the role of the bone in glucose metabolism through its polypeptide osteocalcin (OCN). In this chapter, we will review the role of OCN in diabetes.
WHAT IS OSTEOCALCIN?
Osteocalcin is an essential component of the extracellular matrix of bone. The osteocalcin gene is located on human chromosome 1 (1q25-q31) and is regulated at the transcriptional level by 1,25-dihydroxyvitamin D3 and at post-translational gamma-carboxylation by vitamin K.
Some of the osteocalcin gets partially carboxylated or undercarboxylated (ucOCN or Glu-OCN), which has a low affinity for hydroxyapatite and gets leaked into circulation. This component has been found to have an endocrine role in energy metabolism. The normal level of circulating osteocalcin in serum ranges from 5 to 25 ng/mL.
GAMMA-CARBOXYLATION OF OSTEOCALCIN (FIG. 1)
During post-translational processing, the glutamic acid residues on the osteocalcin prohormone are carboxylated (addition of a COOH group) by the enzyme gamma-glutamyl carboxylase, which requires vitamin K as a cofactor.
Uncarboxylated osteocalcin is also secreted and enters the bloodstream where it has been reported to act on pancreatic B cells to enhance insulin secretion and thus influence glucose metabolism. Of the total amount of OC in circulation, 40–60% is ucOC.
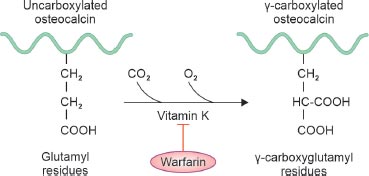
FIG. 1: Vitamin K is required for the formation of carboxyglutamic acid (Gla) is a unique amino acid that is created by vitamin-K-dependent post-translational modification of specific glutamic acid residues in osteocalcin.
UNDERCARBOXYLATION IN HUMANS
In 2007, the Karsenti group was the first to demonstrate that circulating ucOC regulates whole-body energy metabolism via mechanisms that involved increasing insulin secretion from pancreatic β-cells as well as enhancing insulin sensitivity in peripheral tissues. This led to further exploration of the role of this bone-pancreas link and established the endocrine function of this hormone.
GLUCOSE METABOLISM
Osteocalcin and β-cell Function
The β-cells of the pancreatic islets also express G protein-coupled receptor family C group 6 member A (Gprc6a) and the binding of osteocalcin by this receptor activates signaling through the mitogen-activated protein (MAP) kinase pathway increasing insulin secretion. Animals studies involving mice have shown that OCN increases with improved β-cell function. In β-cells, ucOC promotes pancreatic β-cell proliferation and insulin expression and secretion, thus increasing insulin levels. In adipocytes, ucOC induces upregulation of adiponectin, an adipokine that facilitates insulin sensitivity, thereby ameliorating insulin resistance.
Human studies have supported this observation. A study by Huang et al., in Korean diabetics showed that OCN increased β-cell function. This was also proven in a Japanese study. However, there are conflicting results from a Chinese study which does not show this association, as it came up with a negative observation. Whether this is an ethnic variation or an individual characteristic, is not yet known.
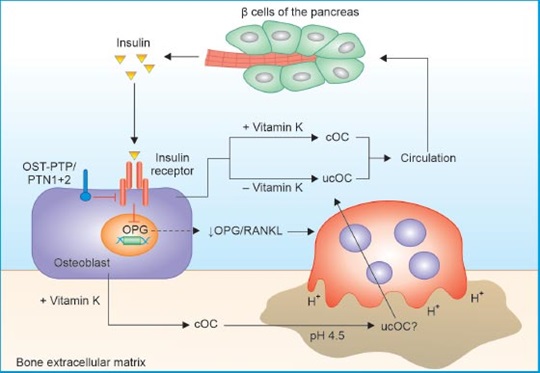
FIG. 2: Speculative model of the role of osteocalcin in glucose metabolism.
(cOC: carboxylated osteocalcin, OPG: osteoprotegerin, ucOC: undercarboxylated osteocalcin)
Osteocalcin and Insulin Resistance
Osteocalcin-deficient mice showed hyperglycemia and glucose intolerance, decreased insulin secretion, decreased insulin sensitivity and adiponectin expression, and increased fat mass and serum triglyceride levels. All of this points to a role for insulin resistance being affected by OCN.
Several human studies have come up analyzing this association. A cross-sectional study, conducted by Sarkar PD et al. on 108 Indians in central India, with newly detected diabetes found a significant negative association of osteocalcin with homeostasis model assessment of insulin resistance (HOMA-IR) (p = 0.001) when compared to healthy controls after linear regression analysis and adjusting with age, gender, body mass index (BMI) and waist-hip ratio. Another study by Weiler et al. on Canadian females showed that insulin resistance (HOMA-IR) has confirmed this negative association (r = −0.21, < 0.0001). It also showed that there was an increase in serum glucagon-like peptide-1 (GLP-1) with an increase in OCN, showing some role for the incretin axis in this association of OCN.
Osteocalcin and Control of Diabetes (Fig. 2)
Glycated hemoglobin levels were found to be lower in patients with higher OCN in Chinese individuals. Several studies have shown that there is a negative correlation between fasting and postprandial sugar and osteocalcin levels in Korean subjects. Further, the duration of diabetes also affects the OCN levels with lower levels seen with longer duration of diabetes. Whether this is a cause or an effect is not clear.
It is also documented that long-term studies of patients diagnosed with diabetes and matched controls indicated that serum total OCN was an independent risk factor for the development of diabetes.
Osteocalcin and Types of Diabetes Mellitus
Osteocalcin levels are different in type 1 diabetes mellitus (T1DM) and T2DM, as the pathophysiologies are totally different. Serum OCN was found to be low in patients with T1DM. So far, in human beings, studies have shown that serum OCN concentration was found to be significantly lower in type 2 diabetic patients than in those with normal glucose tolerance (NGT) and was inversely correlated with insulin resistance (HOMA-IR), fasting plasma glucose (FPG), glycated hemoglobin (HbA1c), and positively correlated with baseline insulin secretion (HOMA-β).
In a study done in South India, Vinay et al. showed OCN levels were lower in patients with increased insulin resistance. Further, it has been shown that OCN prevents and ameliorates β-cell dysfunction. Both these actions contribute to the control of sugars and hence prevent diabetes, and contribute to the control of diabetes. On the contrary, lower levels of OCN can cause an increase in insulin resistance and β-cell dysfunction leading to uncontrolled diabetes.
Osteocalcin and Metabolic Syndrome
Since OCN is known to affect glucose and lipid metabolism through its mechanism of decreasing insulin resistance, it is obvious that it would affect the occurrence of metabolic syndrome.
It has been shown that OCN causes increased levels of leptin, and a decrease in adiponectin. An Egyptian study showed that OCN had a negative correlation with body mass index. However, some Indian studies have not corroborated this finding. Similarly, OCN has been shown to be associated with lower visceral obesity but some studies have shown conflicting results in this area.
Though OCN has minimal effect on blood pressure, it has a significant bearing on lipid metabolism. Higher levels of OCN have been associated with lower triglyceride levels. Ayesha Almas et al. showed that OCN was associated with higher high-density lipoprotein (HDL) levels. Putting all this together, a Chinese study showed that OCN was significantly lower as the components of metabolic syndrome increased.
Osteocalcin and Diabetic Kidney Disease
The bone kidney axis in diabetes may go through OCN and this has a significant effect on complications of diabetes also. Changes in OCN levels have been noted to change with the progression of diabetic nephropathy. Inukai et al. noted higher OCN levels in patients with early Diabetic Nephropathy even before the rise in creatinine. As estimated glomerular filtration rate (eGFR) falls, the OCN levels further rise.
This brings us to the question if rising OCN levels are indeed a biomarker of the progression of kidney disease. The reason for the higher OCN levels could be decreased excretion by a failing kidney or a compensatory increase of OCN for the higher glycemia. The exact mechanism is still unknown, though we know OCN does rise progressively with renal dysfunction. Whether targeting OCN to bring it down, would prevent progression to more severe stages of CKD, is also unknown. This may make it an ideal target for therapeutic intervention to prevent the onset and progression of renal failure.
A definite association of diabetic retinopathy with OCN has not been found, as studies in this area have not been conclusive. However, it has been postulated that OCN may have a role in preventing microvascular complications of DM.
Osteocalcin and Metabolic Dysfunction Associated Fatty Liver Disease
It is well known that metabolic dysfunction-associated fatty liver disease (MAFLD) is associated with T2DM, as part of the metabolic components such as high triglyceride, low HDL, and high-blood pressure with central obesity. The association of MAFLD with OCN was looked at in a Chinese study of 1889 patients. In this study, MAFLD was studied in association with various quartiles of OCN levels. It was shown that increased serum osteocalcin levels are associated with lower occurrence of MAFLD. With the well-known association of OCN causing lower insulin resistance, this is not surprising, as insulin resistance is the theme of all the components of MAFLD. This suggests that OCN can be used as a biomarker for the risk of MAFLD in T2DM.
It was also demonstrated that OCN levels were associated with lower levels of AST and ALT suggesting that liver injury is mitigated by OCN. Further, inflammation is at the center of the pathophysiology of MAFLD. This is associated with higher CRP levels and can translate in the future into varying degrees of cirrhosis. It is well known that OCN is inversely proportional to levels of inflammatory markers, such as C-reactive protein (CRP) and ferritin. This may be a mechanism by which OCN reduces MAFLD. Thus, OCN levels may help to predict, degrees of MAFLD, and the chances of progression to further inflammation and fibrosis.
Osteocalcin and Vascular Complications
It has been proposed that osteocalcin can ameliorate endothelial dysfunction through an insulin-sensitizing effect. It is said to stimulate the phosphatidylinositol 3-kinase (PI3-kinase)/Akt signaling pathway.
The role of OCN in vascular complications has been controversial. Several studies have shown that OCN may be related to endothelial dysfunction and vascular calcification; however, none of these have been conclusive. The association with vascular dysfunction is more evident in postmenopausal women and this has led to the theory that there may be some difference between the sexes as far as the role of OCN is concerned.
In a meta-analysis of 31 observational studies involving 21,000 patients, it was found that there was an inverse relationship between aortic and coronary classification and carotid intima-media thickness and OCN levels. The only problem with this data was that most of the studies were cross-sectional and observational. There have been conflicting reports on the role of OCN on vascular health, and the last word on this is still not clear.
Osteocalcin and Atherosclerosis
There have been studies showing the association of OCN and atherosclerosis. In patients with chronic kidney disease, the carotid intima media thickness was measured by Zhang et al. In a study done in postmenopausal women decreased OCN was associated with greater arteriosclerosis.
The risk of coronary atherosclerosis by calculating coronary artery calcium in patients who underwent coronary artery bypass graft (CABG) was found to be higher, with lower levels of OCN. There have been no major studies in India documenting the association between OCN and atherosclerosis.
IS OCN A TARGET FOR PREVENTION OF DIABETES?
It is well known that OCN is inversely correlated to insulin resistance, and this makes it an attractive target for therapeutic purposes. It is interesting to note that 8 weeks of aerobic training in young obese individuals, increases OCN levels significantly, along with bringing down body fat, especially the visceral component. Insulin sensitivity also increased showing that the mechanism of this change, had a role in insulin resistance. This brings up the question if OCN can be used to quantify the risk of developing diabetes. Further, can we assess the efficacy of a lifestyle modification on glucose metabolism, by measuring OCN, is also an interesting idea.
CONCLUSION
To conclude, given the effects of OCN on glucose metabolism, it is tempting to suggest that OCN may be a drug for the control of DM, if it can be modified to a consumable form. Research is ongoing in this area, and like several therapeutic targets for diabetes which have evolved, over the last decade, this too may be a drug for the future.
SUGGESTED READINGS
1. Lacombe J, Al Rifai O, Loter L, Moran T, Turcotte AF, Grenier-Larouche T, et al. Measurement of bioactive osteocalcin in humans using a novel immunoassay reveals association with glucose metabolism and β-cell function. Am J Physiol Endocrinol Metab. 2020;318(3):E381-91.
2. Zhang Y, Zhou P, Kimondo JW. Adiponectin and osteocalcin: relation to insulin sensitivity. Biochem Cell Biol. 2012;90(5):613-20.
3. Weiler HA, Lowe J, Krahn J, Leslie WD. Osteocalcin and vitamin D status are inversely associated with homeostatic model assessment of insulin resistance in Canadian Aboriginal and white women: the First Nations Bone Health Study. J Nutr Biochem. 2013;24(2):412-8.
4. Kumar V, Bolanthakodi N, Vidyasagar S, Holla A, Sheik SM, Abhishek S. Association of serum osteocalcin with beta cell function, insulin resistance, and glycemic parameters in south Indian type 2 diabetic subjects. Int J Diabetes Dev Ctries. 2023;43:469-75.
5. Guo X, Li Y, Zhou Y, Zhang C, Liang S, Zheng Y, et al. Osteocalcin association with vascular function in chronic kidney disease. J Clin Hypertens (Greenwich). 2022;24(7):928-36.
6. Yang M, Luo S, Yang J, Chen W, He L, Liu D, et al. Bone-kidney axis: A potential therapeutic target for diabetic nephropathy. Front Endocrinol (Lausanne). 2022;13:996776.
7. Wang YJ, Jin CH, Ke JF, Wang JW, Ma YL, Lu JX, et al. Decreased Serum Osteocalcin is an Independent Risk Factor for Metabolic Dysfunction-Associated Fatty Liver Disease in Type 2 Diabetes. Diabetes Metab Syndr Obes. 2002;15:3717-28.
8. Tacey A, Hayes A, Zulli A, Levinger I. Osteocalcin and vascular function: is there a cross-talk? Mol Metab. 2021;49:101205.
9. Millar SA, Patel H, Anderson SI, England TJ, O’Sullivan SE. Osteocalcin, vascular calcification, and atherosclerosis: a systematic review and meta-analysis. Front Endocrinol (Lausanne). 2017;8:183.
 Home
Home
e-Contents
Chapter 1e: Prosthetic Valve Thrombosis
Harbir Kaur Rao, Rajinder Singh GuptaChapter 2e: Diabesity and Glucagon-like Peptide-1 Receptor Agonists
Rajiv Awasthi, Avivar AwasthiChapter 4e: Gestational Diabetes Mellitus: An Update
Vinay Kumar Meena, Nazim Hussain, Rajani NawalChapter 5e: Sodium-glucose Cotransporter-2 Inhibitors Beyond Glycemia
Amit VarmaChapter 6e: Intrahepatic Cholestasis
Archith Boloor, Nikhil Kenny ThomasChapter 8e: Tobacco and Chest
Rajbir Singh, Prabhpreet Kaur, BL Bhardwaj, RS BhatiaChapter 9e: Lung Metastasis
RS Bhatia, Prabhpreet Kaur, Rajbir Singh, BL BhardwajChapter 10e: Important Drug Interactions in Clinical Practice
Srirang AbkariChapter 11e: Renal Tubular Acidosis
Surjit TarafdarChapter 12e: Anemia in Chronic Kidney Disease
Saif Quaiser, Ruhi Khan, Shahzad Faizul HaqueChapter 14e: Current Positioning of Nonstatin Therapy of Dyslipidemia
Saumitra Ray, Srina RayChapter 15e: How to Deal with Complication of Prolonged Antibiotic Therapy
Pushpita MandalChapter 16e: Navigating End-of-life Medical Decisions with Cultural Sensitivity
Reinold OB GansChapter 17e: Osteocalcin: New Frontiers in Diabetes
Sudha Vidyasagar, Avinash HollaChapter 18e: Arterial Blood Gas Analysis: A Rational Approach
SV Ramanamurty, TVSP MurtyChapter 19e: Asthma: New Therapeutic Avenues
Sachin Hosakatti